Introduction
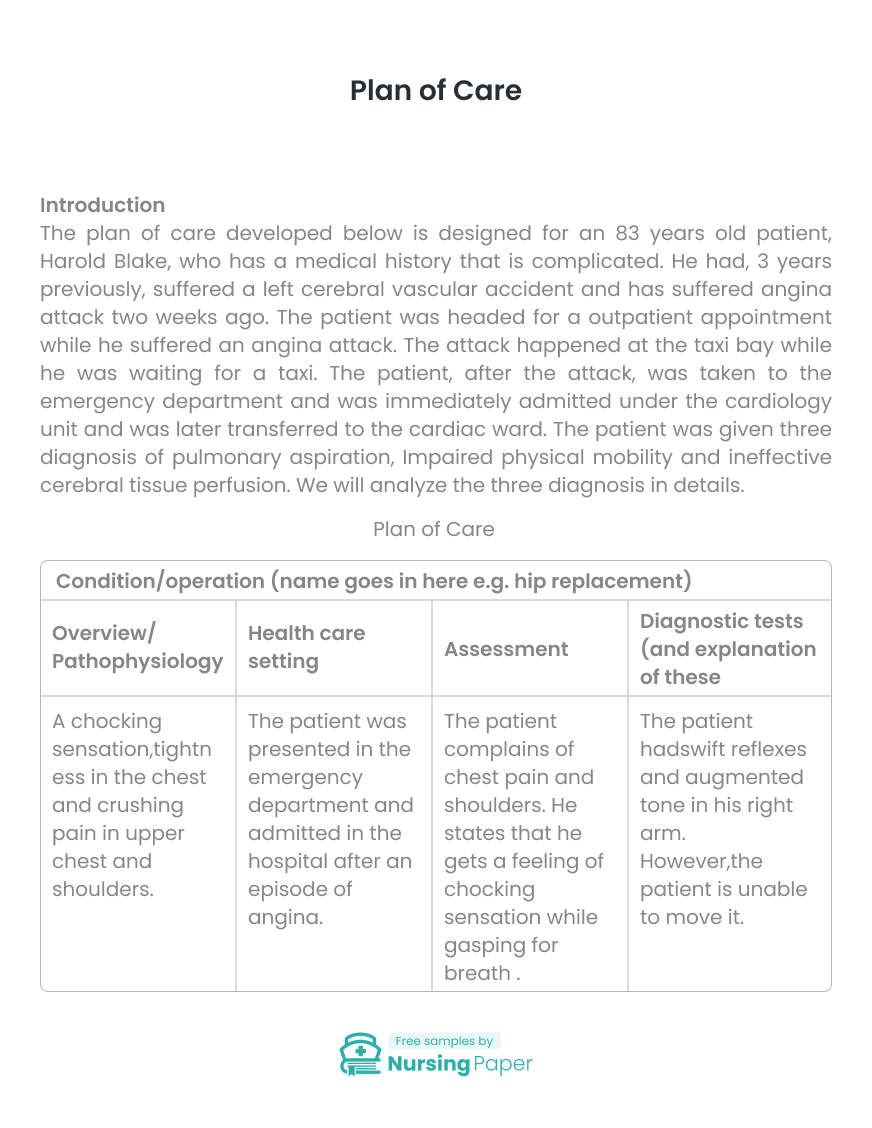
The plan of care developed below is designed for an 83 years old patient, Harold Blake, who has a medical history that is complicated. He had, 3 years previously, suffered a left cerebral vascular accident and has suffered angina attack two weeks ago. The patient was headed for a outpatient appointment while he suffered an angina attack. The attack happened at the taxi bay while he was waiting for a taxi. The patient, after the attack, was taken to the emergency department and was immediately admitted under the cardiology unit and was later transferred to the cardiac ward. The patient was given three diagnosis of pulmonary aspiration, Impaired physical mobility and ineffective cerebral tissue perfusion. We will analyze the three diagnosis in details.
Pulmonary Aspiration
Pulmonary aspiration is the entry of materials from the gastrointestinal tract into the lower respiratory system. The foreign materials may be inhaled or delivered into the trachea system Nason, 2015). When pulmonary aspiration occurs during feeding, then it is considered as food going down the wrong pipe. Pulmonary aspiration symptoms include coughing, difficulty in breathing and in some cases the patient can exhibit signs of chocking. In our case, the patient, Harold Blake, upon admission showed the symptoms of choking, shortness of breath, crushing pain in the upper chest and chest tightness. The symptoms that the patient showed were similar to those of pulmonary aspiration and thus it was rational to diagnose the disease since it could be a possibility.


The nurse should evaluate the ability of the patient to swallow by assessing for chocking, coughing, throat clearing and the presence of a wet voice during and or after swallowing. The nurse should also check for residual food in the mouth after eating( Marik, 2011). The reason for this assessment is because dysfunctional swallowing multiplies the aspiration risk. There is still a need for legitimate and easy-to-use methods that could be used to screen for aspiration risk. The nurse should access the presence of nausea or vomiting. The assessment is necessary because nausea puts the patients at a higher risk of aspiration and more so if the level of awareness is compromised. The head of patient’s bed raised when the patient is feeding and half an hour after feeding. The reason for this intervention is the maintenance of a sitting position during and after eating help in decreasing the aspiration pneumonia, especially in elderly people.
The evaluation of the ability of the patient to swallow would help accomplish a short-term goal of enabling the health provider to determine if the patient is suffering from impaired swallowing. This would enable the health provider to assist the patient in swallowing should they have a problem. The assessment of the presence of nausea and vomiting in the patient during feeding helps achieve a short-term objective of stopping aspiration (Green, Mason, & Krauss, 2017). The determination of the of whether the consciousness of the patient is compromised works well in controlling the aspiration. The practice of sitting in an elevated manner for the patient will aid in achieving the longterm gains of decreasing the chances of recurrence of the aspiration since its an intervention that should be carried on even after discharge.
Impaired Physical Mobility
Impaired physical mobility is the restriction in the self-reliant physical motion of the body or one of the functions of the body. When impaired physical mobility happens, it can turn to be a complex health issue that involves different healthcare team. The happening of this disease continues to rise with the increase in the age of an individual. After discharge from hospitals in most cases, the patient is moved to a rehabilitation center or goes home with a physical therapy (Wu, Han, Xu, Lu, Cong, Zheng, & Sun, 2014). In this case, the patient had previously suffered a left cerebral vascular accident. Upon admission, the doctor had noted that he was drowsy, drooling, and is having difficulty speaking. Upon observation, the patient ’s right limbs were moderately weak and sluggish as compared to their left counterparts which were possible leads to impaired physical mobility.

The doctor could make the patient walk around at a regular pace. The patient could have one flight or more. However, during the flight, the patient should have more short of breath than normal. Then the patient could walk about one street block that is on the level and climb one flight without stopping. After that, the patient walks for 50 feet without stopping and climb one flight of stairs without stopping. The aim of this assessment is to understand the particular levels of the impairment. This understanding helps to guide the design of the best management plan. The nurse should assess the nutritional needs of the patients as they are directly related to the immobility. The correct nutrition would give the patient the required energy to participate in the required activities that are necessary for the rehabilitation. The nurse should also evaluate the level of the pain related to exercise and the changes in the joint mobility. The aim of this is to examine the development of recession of the complications. The assessment would give the nurse the indication as to whether the exercise should delay or stop until further healing occurs.
The procedure of making the patient walk around in distances that keep reducing with time and depending on the ability of the patient to go on helps in creating a short-term objective of identifying those parts of the body that are affected as well as determining the extent to which the impairment has reached (Crawford, & Harris, 2016). Identifying the stage of the impairment is crucial in determining the short-run measure to be adopted. The nutritional evaluation is also important in short-run as it determines the kind of diet that the patient should adopt in order to get enough energy to carry on with the exercises. The nutritional determination also plays a big part in the long-term rehabilitation of the patient until they fully recover. The assessment of the pain degree determines the long-term exercises that would be suitable for the patient on their journey to recovery.
Ineffective Cerebral Tissue Perfusion
Ineffective cerebral tissue perfusion is as a result of decreased oxygen supply resulting from failure to supply tissues at the capillary level. The ineffective cerebral tissue perfusion results from the insufficient flow of blood in arteries which causes decreased movement of nutrients and oxygen to the cellular level (Hasanin, Mukhtar, & Nassar, 2017). This conditions could be short-lived with few effects on the health of the patient but it could also be chronic. When Ineffective cerebral tissue perfusion becomes degenerative, it could consequence in tissue and organ damage or even death. The patient, in this case, showed symptoms of pain in the chest, chest retraction, change in motor response, speech abnormalities and nausea. These symptoms are same as those of the Ineffective cerebral tissue perfusion.



The nurse should access the decreased tissue perfusion. This is because most of the signs of the Ineffective cerebral tissue perfusion are common to other illnesses. Therefore the evaluation provides a baseline for future comparisons. The doctor review laboratory data if medication is used for treatment. The doctor should also determine if anticoagulants have been used for treatment. This is because studies on blood clotting are used to resolve or ensure that clotting factors remain within curative levels. Irregularities in clotting may occur as an effect of curative measures. The diagnostic tests should be submitted as indicated as there are various tests available and they depend on the reason of the impaired tissue.
The assessment of the decreased tissue perfusion gives a short-term goal of identifying with certainty the cause of the tissue perfusion. The laboratory tests also form the bases for the short-term goal of stabilizing the condition (Iskhandar, & Christensen, 2012). It also creates a base for the long-term goal of controlling the ailment and conquering it completely.
Legal and Ethical Consideration
The patient in this case was attacked by angina while on a taxi bay where he received assistance and taken to hospital. There are laws in place that protect the good Samaritans who assist individual in danger from being prosecuted for causing injury to the person. The law encourages persons to offer acts of helping persons in need. The healthcare providers in duty are also allowed to attend to the patient once presented in hospital. However they must seek the consent of the injured person. Some situations however do not need consent, especially if the patient is not in a position to offer the consent.
Inter-Professional Consideration
For Ineffective cerebral tissue perfusion, the professionals involved would be a lab technician for carrying out the lab tests, a nurse for taking care of the patient and cardiologist. For Impaired physical mobility, an exercise therapist would be required. The main health staff that would be essential for this patient is a cardiologist. This is because the patient was admitted for an angina attack. Angina in itself is not a disease but rather a symptom of a cardiovascular condition (Manolis, Poulimenos, Ambrosio, Kallistratos, Lopez-Sendon, Dechend, Mancia, & Camm, 2016).
Ineffective cerebral tissue perfusion is also concerned with a cardiovascular condition that involves the limited flow of blood to the necessary tissues. According to (Mckenna & Sugrue, 2015) the cardiologist would give treatment that would be intended to reduce the pain and prevent a heart attack. For this patient, the cardiologist is likely to offer nitrate medicines which cut down the magnitude of angina attacks by relaxing and widening blood vessels. He is also likely to recommend to the patient to control their weight, a lot of resting, avoid large volumes of meals, change their diet, regular checking of cholesterol levels and stress management.
Conclusion
Angina and heart-related problems are common issues that require the patient to always be aware of themselves as well as taking good care of themselves. The nursing care is a credible criterion for diagnosing the patient as well as stabilizing the patient. Proper adherence to the nursing plan would see a quick recovery of the patient.
1. Crawford A., & Harris, H. (2016). Caring for adults with impaired physical mobility. Nursing. 46, 36-41.
2. Green SM, Mason KP, & Krauss BS. (2017). Pulmonary aspiration during procedural sedation: a comprehensive systematic review. British Journal of Anaesthesia. 118, 344-354.
3. Hasanin, A., Mukhtar, A., & Nassar, H. (2017). Perfusion indices revisited. Journal of Intensive Care. 5.
4. Iskhandar Shah, L., & Christensen, M. (2012). Ineffective cerebral perfusion related to increased intracranial pressure secondary to subarachnoid haemorrhage: An examination of nursing interventions. Singapore Nursing Journal. 39, 15-24.
5. Manolis, A. J., Poulimenos, L. E., Ambrosio, G., Kallistratos, M. S., Lopez-Sendon, J., Dechend, R., Mancia, G., & Camm, A. J. (2016). Medical treatment of stable angina: A tailored therapeutic approach. International Journal of Cardiology. 220, 445-453.
6. Marik PE. (2011). Pulmonary aspiration syndromes. Current Opinion in Pulmonary Medicine. 17, 148-54.
7. Mckenna CJ, & Sugrue DD. (2015). The medical management of chronic stable angina. National Institute of Health 38, 131-136
8. Nason, K. S. (2015). Acute Intraoperative Pulmonary Aspiration. Thoracic Surgery Clinics. 25, 301-307.



The download will start shortly.

The download will start shortly.
 Subject:
Medicine
Subject:
Medicine  Number of pages: 4
Number of pages: 4  Subject:
Health and Social Care
Subject:
Health and Social Care  Number of pages: 2
Number of pages: 2  Subject:
Health and Social Care
Subject:
Health and Social Care  Number of pages: 9
Number of pages: 9  Subject:
Medicine
Subject:
Medicine  Number of pages: 3
Number of pages: 3  Subject:
Medicine
Subject:
Medicine  Number of pages: 6
Number of pages: 6  Subject:
Nursing
Subject:
Nursing  Number of pages: 5
Number of pages: 5  Subject:
Nursing
Subject:
Nursing  Number of pages: 4
Number of pages: 4  Subject:
Medicine
Subject:
Medicine  Number of pages: 2
Number of pages: 2  Subject:
Medicine
Subject:
Medicine  Number of pages: 13
Number of pages: 13  Subject:
Health and Social Care
Subject:
Health and Social Care  Number of pages: 2
Number of pages: 2  Subject:
Nursing
Subject:
Nursing  Number of pages: 2
Number of pages: 2  Subject:
Health and Social Care
Subject:
Health and Social Care  Number of pages: 4
Number of pages: 4  Subject:
Medicine
Subject:
Medicine  Number of pages: 8
Number of pages: 8  Subject:
Health and Social Care
Subject:
Health and Social Care  Number of pages: 2
Number of pages: 2  Subject:
Nursing
Subject:
Nursing  Number of pages: 8
Number of pages: 8 
